ECT and Radiology- a New Finding
Out on PubMed, from researchers at Vanderbilt University School of Medicine, in Nashville, Tennessee, is this case report:
Chronic Electroconvulsive Therapy May Induce Calvarial Hyperemia and Marrow Replacement.
J ECT. 2020 Oct 27. doi: 10.1097/YCT.0000000000000728. Online ahead of print.PMID: 33122499
The abstract is copied below:
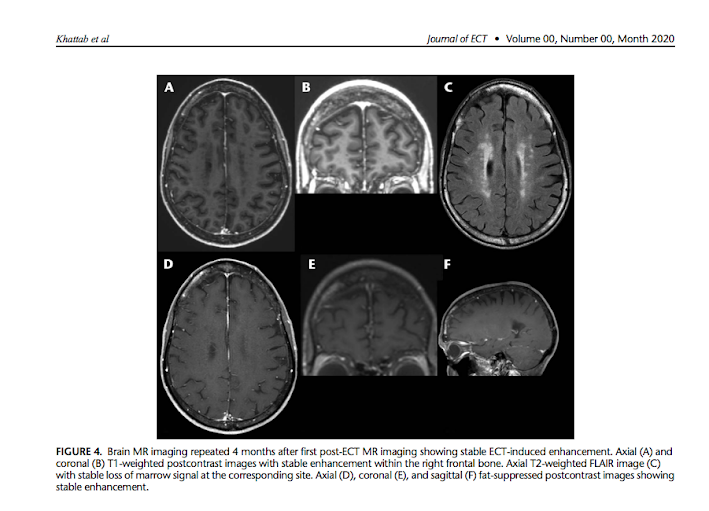
Electroconvulsive therapy (ECT) is a treatment option for a number of psychiatric disorders, including refractory major depression and obsessive compulsive disorder. There are no known structural sequelae of ECT. Here we present a patient with severe refractory obsessive compulsive disorder and major depression treated over 2 years with ECT every 2 weeks. Planning magnetic resonance imaging intended for a potential procedural intervention for her psychiatric disease incidentally demonstrated a new area of increased enhancement and loss of marrow signal within the right frontal bone. Imaging findings were suggestive of underlying bone marrow or bone changes, although there was no evidence of bone destruction on bone-windowed computed tomography (CT) and there was no uptake on nuclear bone scan. The CT chest/abdomen/pelvis were also reassuring that this did not represent metastatic disease, and findings were unchanged on repeat magnetic resonance imaging 4 months later. Thus, this area corresponded to the site directly underlying the unilateral ECT electrode placement, suggestive of never-before described ECT-induced hyperemia. We report for the first time that frequent, chronic ECT may induce asymptomatic skull bone marrow hyperemia with radiologic findings. This appears to be a direct consequence of electrical current leading to chronic inflammatory and edematous marrow replacement. Electroconvulsive therapy should be added to the neuroradiological differential diagnosis of calvarial enhancement and loss of marrow signal. Psychiatrists should counsel patients on the possibility of this rare radiological finding, which may be confused for other processes.And from the text:
It is surprising, if this finding is truly associated with the ECT that the patient received, that it has never been noticed before. A radiologist friend of mine was kind enough to review the images in the case report, and found them convincing.
The patient in this case was a 71 year-old woman with severe OCD and depression who got the MRI as part of the workup for a radiosurgical capsulotomy to treat her OCD. Further follow up about her clinical status would be very instructive...


Comments
Post a Comment