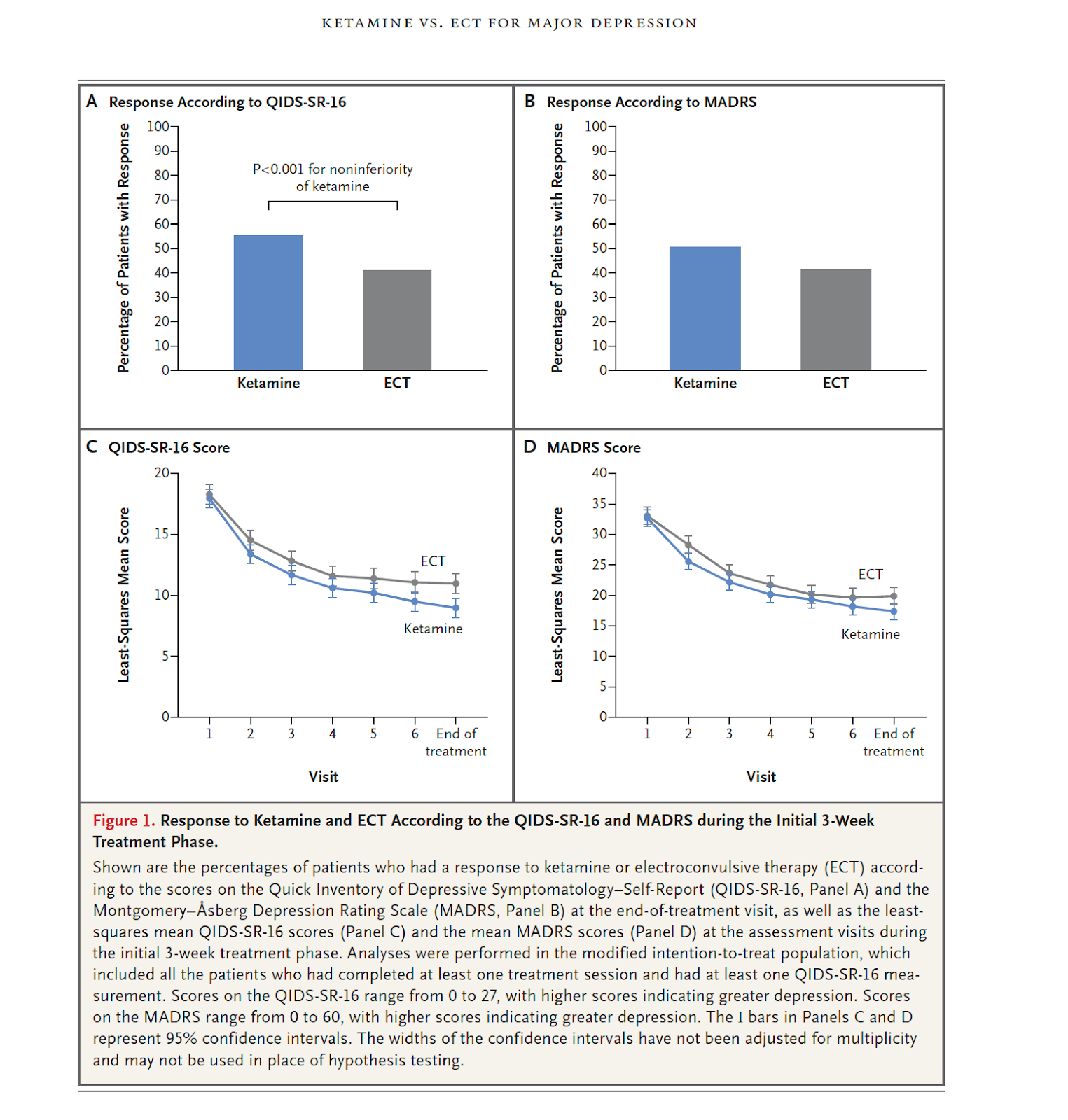
Out on PubMed, from investigators in the US, is this study: Ketamine versus ECT for Nonpsychotic Treatment-Resistant Major Depression. Anand A, Mathew SJ, Sanacora G, Murrough JW, Goes FS, Altinay M, Aloysi AS, Asghar-Ali AA, Barnett BS, Chang LC, Collins KA, Costi S, Iqbal S, Jha MK, Krishnan K, Malone DA, Nikayin S, Nissen SE, Ostroff RB, Reti IM, Wilkinson ST, Wolski K, Hu B. N Engl J Med. 2023 May 24. doi: 10.1056/NEJMoa2302399. Online ahead of print. PMID: 37224232 The abstract is copied below: Background: Electroconvulsive therapy (ECT) and subanesthetic intravenous ketamine are both currently used for treatment-resistant major depression, but the comparative effectiveness of the two treatments remains uncertain. Methods: We conducted an open-label, randomized, noninferiority trial involving patients referred to ECT clinics for treatment-resistant major depression . Patients with treatment-resistant major depression without psychosis were recruited and assigned in a 1:1 rat