"Anticholinergic Burden," Cognition and ECT: New Study From France
Out on PubMed, from investigators in France, is this paper:
The anticholinergic burden is not associated with cognitive impairments in patients treated by electroconvulsive therapy for treatment-resistant depression.
J Psychiatr Res. 2022 Mar 24;150:87-95. doi: 10.1016/j.jpsychires.2022.03.038. Online ahead of print. PMID: 35366599
The abstract is copied below:
Background: Electroconvulsive therapy (ECT) is the most effective non-pharmacological treatment for treatment-resistant depression (TRD) but can expose to transient cognitive impairments. Understanding factors underlying these cognitive side effects is important. This study investigated the impact of anticholinergic treatments on cognitive performances after ECT courses for TRD in naturalistic condition.
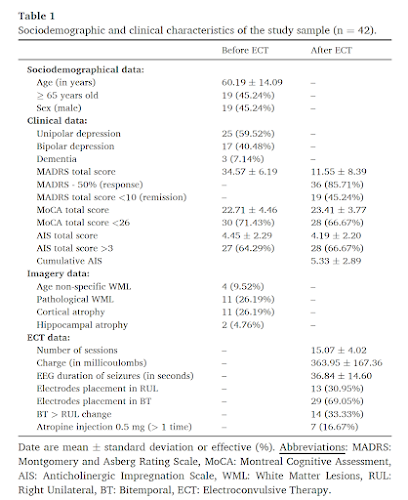
Methods: Impact of anticholinergic burden (Anticholinergic Impregnation Scale, AIS) on cognitive changes (Montreal Cognitive Assessment, MoCA) adjusted on depression level (Montgomery and Asberg Depression Scale, MADRS) was investigated in 42 patients who received an ECT course between 2017 and 2020 for unipolar or bipolar TRD. Collection of daily treatments given during ECT was carried out via the computerized traceability of treatments validated by nurses.
Results: Among the 31 treatments identified with an anticholinergic score, which represent only 38% of total treatments, the three most frequently given treatments were Lorazepam (47%), Venlafaxine (36%) and Cyamemazine (26%). Delayed recall was the most frequently impaired cognitive function after ECT courses. Using logistic regression, we found no association between the anticholinergic burden and the decrease in cognitive scores after ECT courses, adjusted on MADRS score evolution (p > 0.1). Conversely, improvement in MADRS scores were correlated with improvement in attention MoCA subscores.
Limitations: This is a retrospective monocentric study with a moderate sample size using anticholinergic scales to calculate the anticholinergic burden without plasma dosage.
Conclusion: Anticholinergic treatments did not seem to explain ECT-related cognitive impairments. This warrants further large prospective investigations including different measures of anticholinergic burden.
Keywords: Anticholinergic burden; Cholinergic antagonists; Cognitive dysfunction; Depression; Electroconvulsive therapy.
The paper is here.
And from the text:
Anticholinergic burden and cognitive outcome in ECT seems like an interesting topic to investigate. Unfortunately, the methodological shortcomings of this study (retrospective chart review, use of only the MoCA for cognitive assessment, no direct measurement of anticholinerginicity) pretty much doom it to failure.
A good theoretical idea, good literature review and discussion, good clinical advice to avoid anticholinergic meds in older patients, and a lovely Fig. 1 are all here, despite no definitive results.
Kudos to our French colleagues for this effort and for their ongoing research to further refine ECT.





Comments
Post a Comment