Review of Treatments For Postictal Agitation in ECT
Out on PubMed, from investigators in the Netherlands, is this review:
Pharmacological prevention of postictal agitation after electroconvulsive therapy-A systematic review and meta-analysis.
Front Psychiatry. 2023 Apr 20;14:1170931. doi: 10.3389/fpsyt.2023.1170931. eCollection 2023.PMID: 37151968

Background: Postictal agitation (PIA) after electroconvulsive therapy (ECT) is a serious clinical problem estimated to occur in 7-36% of patients and recur in 19-54% of patients. PIA has the potential to cause dangerous situations for the patient and staff members aside from the financial impact. To date, it is unclear which pharmacological interventions should be used in the management of PIA. This study aimed to systematically review the (preventative) pharmacological treatment options for PIA after ECT.
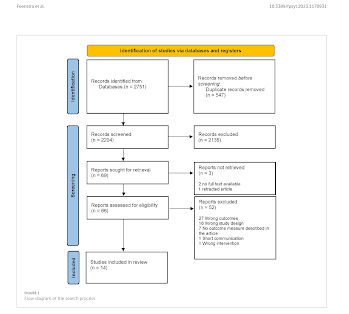
Method: A systematic search was done in PubMed, EMBASE, PsycINFO, and Web of Science from inception until 10 November 2022. We included randomized trials with any pharmacological intervention or comparison and a predefined outcome measure on PIA. Studies that solely included patients with neurodegenerative disorders or stroke were excluded. Data quality was assessed with the RoB2 and GRADE. Meta-analysis was performed if possible. This study was registered on PROSPERO under CRD42021262323.
Results: We screened 2,204 articles and included 14 studies. Dexmedetomidine was investigated in 10 studies. Alfentanil, lignocaine, esmolol, midazolam, propofol, ketamine, haloperidol, and diazepam were each studied in only one study. Meta-analysis revealed an OR of 0.45 (0.32-0.63), a moderate effect size, in favor of dexmedetomidine than placebo to prevent PIA with very low heterogeneity (I2 = 0%). The certainty of the evidence was moderate. The other interventions studied were all found to have low certainty of evidence.
Conclusion: For clinical practice, we believe that our results indicate that dexmedetomidine should be considered for the prevention of PIA in patients that have previously experienced PIA.
Keywords: ECT; cognitive side effects; dexmedetomidine; electroconvulsive therapy; postictal agitation.
The article is here.
And from the text:
Well, managing and preventing postictal agitation is important, and dexmedetomidine is a very good and interesting drug....but this review seems to depart from common sense and tried and true clinical experience. PIA is well managed in most (admittedly, not all) cases by either midazolam of propofol, and more easily so. Again, dexmedetomidine is a remarkable drug, but its rightful place in various aspects of ECT anesthesia management is yet to be determined. The systematic review and meta-analysis is academically sound, but somewhat a case of "garbage in, garbage out" because of the nature of the literature.




This is a great study on treatment options for PIA. It is a shame, however, that there is no discussion of how PIA develops in the first place and how it might be avoided. I am still convinced that PIA is caused by an insufficient amount of anesthetic or anesthetic depth (see Indian studies of unmodified ECT and PIA rates up to 50%). I still remember that editors of a very renowned journal for anesthesia rejected our paper in this regard with the words that they could not publish it, because EVERY anesthesiologist has known for a long time that PIA results from anesthesia with too low anesthetic doses. Fortunately, we were able to publish our idea in J ECT: Kranaster L, Janke C, Hoyer C, Sartorius A. Management of severe postictal agitation after electroconvulsive therapy with bispectrum electroencephalogram index monitoring: a case report. J ECT. 2012 Jun;28(2):e9-10. doi: 10.1097/YCT.0b013e31823d2fef.
ReplyDelete