Continuation/Maintenance ECT Lowers Readmissions and Costs: New Study From Singapore and Australia
Out on PubMed, from investigators in Singapore and Australia, is this paper:
The association between outpatient continuation/maintenance electroconvulsive therapy, readmission risk and total direct cost in patients with depressive, bipolar and psychotic disorders: A naturalistic retrospective cohort study.
J Affect Disord. 2023 Jun 7:S0165-0327(23)00772-3. doi: 10.1016/j.jad.2023.06.016. Online ahead of print.PMID: 37295655
The abstract is copied below:
Background: The transdiagnostic effect of continuation/maintenance ECT (CM-ECT) across mood and psychotic disorders on hospital psychiatric readmission risk and total direct cost remains unclear.
Methods: A naturalistic retrospective analysis of 540 patients who received inpatient acute ECT treatment from May 2017 to Mar 2021 in a tertiary psychiatric institution. Patients were assessed with validated clinical rating scales pre-ECT and after the first 6 treatments of a course of inpatient acute ECT. After discharge, patients who continued with CM-ECT were compared with those not receiving CM-ECT using survival analysis of hospital readmission. Total direct cost (hospitalisation and ECT treatment cost) was also analysed. All patients were subjected to a standard post-discharge monitoring program with case managers checking in on the patients regularly after discharge and ensuring they were given an outpatient appointment within a month of discharge.
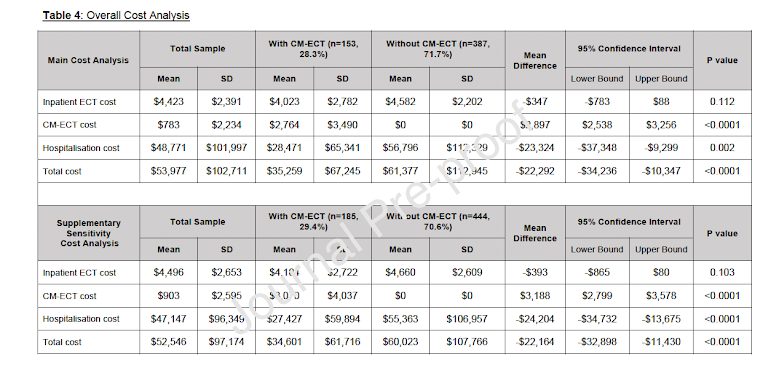
Results: Both cohorts had significant improvement in their rating scales scores after their first six 6 sessions of inpatient acute ECT. Patients who continued with CM-ECT after completing their inpatient acute ECT (mean number of acute ECT: N = 9.9, SD 5.3), had a significantly lower risk of readmission [adjusted hazard ratio of 0.68 (95 % CI: 0.49-0.94, p = 0.020)]. Patients who received CM-ECT also had a significantly lower average total direct cost compared to those who did not (SGD$35,259 vs SGD$61,337). For patients with mood disorders, the CM-ECT group had a significantly lower inpatient ECT cost, hospitalisation cost and total direct costs compared to those without CM-ECT.
Limitations: The naturalistic study cannot prove a causal relationship between CM-ECT and reduced readmission and lower healthcare costs.
Conclusion: CM-ECT is associated with lower readmission risks and lower total direct healthcare costs for the treatment of mood and psychotic disorders, especially for mood disorders.
Keywords: Bipolar; Cost; Depression; Electroconvulsive therapy; Psychotic disorder; Readmission.
Methods: A naturalistic retrospective analysis of 540 patients who received inpatient acute ECT treatment from May 2017 to Mar 2021 in a tertiary psychiatric institution. Patients were assessed with validated clinical rating scales pre-ECT and after the first 6 treatments of a course of inpatient acute ECT. After discharge, patients who continued with CM-ECT were compared with those not receiving CM-ECT using survival analysis of hospital readmission. Total direct cost (hospitalisation and ECT treatment cost) was also analysed. All patients were subjected to a standard post-discharge monitoring program with case managers checking in on the patients regularly after discharge and ensuring they were given an outpatient appointment within a month of discharge.
Results: Both cohorts had significant improvement in their rating scales scores after their first six 6 sessions of inpatient acute ECT. Patients who continued with CM-ECT after completing their inpatient acute ECT (mean number of acute ECT: N = 9.9, SD 5.3), had a significantly lower risk of readmission [adjusted hazard ratio of 0.68 (95 % CI: 0.49-0.94, p = 0.020)]. Patients who received CM-ECT also had a significantly lower average total direct cost compared to those who did not (SGD$35,259 vs SGD$61,337). For patients with mood disorders, the CM-ECT group had a significantly lower inpatient ECT cost, hospitalisation cost and total direct costs compared to those without CM-ECT.
Limitations: The naturalistic study cannot prove a causal relationship between CM-ECT and reduced readmission and lower healthcare costs.
Conclusion: CM-ECT is associated with lower readmission risks and lower total direct healthcare costs for the treatment of mood and psychotic disorders, especially for mood disorders.
Keywords: Bipolar; Cost; Depression; Electroconvulsive therapy; Psychotic disorder; Readmission.
The article is here.
And from the text:



Comments
Post a Comment