ECT vs Ketamine: NEJM Article Sets Up False Equivalency
Out on PubMed, from investigators in the US, is this study:
Ketamine versus ECT for Nonpsychotic Treatment-Resistant Major Depression.
Background: Electroconvulsive therapy (ECT) and subanesthetic intravenous ketamine are both currently used for treatment-resistant major depression, but the comparative effectiveness of the two treatments remains uncertain.
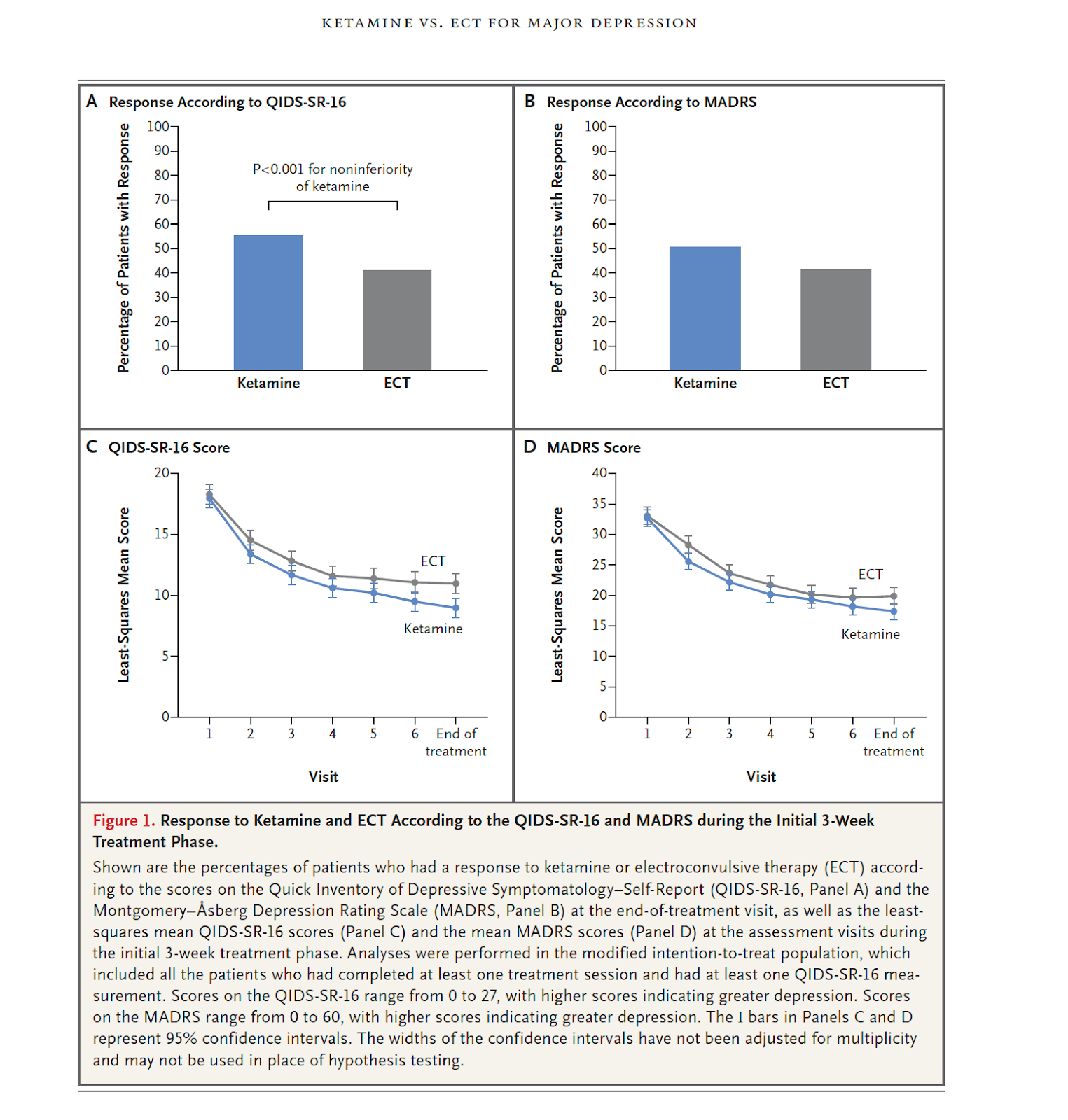
Methods: We conducted an open-label, randomized, noninferiority trial involving patients referred to ECT clinics for treatment-resistant major depression. Patients with treatment-resistant major depression without psychosis were recruited and assigned in a 1:1 ratio to receive ketamine or ECT. During an initial 3-week treatment phase, patients received either ECT three times per week or ketamine (0.5 mg per kilogram of body weight over 40 minutes) twice per week. The primary outcome was a response to treatment (i.e., a decrease of ≥50% from baseline in the score on the 16-item Quick Inventory of Depressive Symptomatology-Self-Report; scores range from 0 to 27, with higher scores indicating greater depression). The noninferiority margin was -10 percentage points. Secondary outcomes included scores on memory tests and patient-reported quality of life. After the initial treatment phase, the patients who had a response were followed over a 6-month period.
Results: A total of 403 patients underwent randomization at five clinical sites; 200 patients were assigned to the ketamine group and 203 to the ECT group. After 38 patients had withdrawn before initiation of the assigned treatment, ketamine was administered to 195 patients and ECT to 170 patients. A total of 55.4% of the patients in the ketamine group and 41.2% of those in the ECT group had a response (difference, 14.2 percentage points; 95% confidence interval, 3.9 to 24.2; P<0.001 for the noninferiority of ketamine to ECT). ECT appeared to be associated with a decrease in memory recall after 3 weeks of treatment (mean [±SE] decrease in the T-score for delayed recall on the Hopkins Verbal Learning Test-Revised, -0.9±1.1 in the ketamine group vs. -9.7±1.2 in the ECT group; scores range from -300 to 200, with higher scores indicating better function) with gradual recovery during follow-up. Improvement in patient-reported quality-of-life was similar in the two trial groups. ECT was associated with musculoskeletal adverse effects, whereas ketamine was associated with dissociation.
Conclusions: Ketamine was noninferior to ECT as therapy for treatment-resistant major depression without psychosis. (Funded by the Patient-Centered Outcomes Research Institute; ELEKT-D ClinicalTrials.gov number, NCT03113968.).
The paper is here.
And from the text:
This paper, timed for release by the NEJM with the APA annual meeting, has, indeed, caused quite a splash in the ECT community, not to mention in the lay press. There is an accompanying editorial, which will be the subject of a future blog post.
There are substantial problems with the conclusion highlighted in yellow above. Without putting this statistical statement into clinical context, the conclusion is misleading.
There are problems with the study design, implementation and reporting. The ECT response/remission rates are astoundingly low and the patient population is younger and more comorbidly ill than a typical ECT population.
It would have been more responsible for the authors to have included several paragraphs in the discussion about how these findings should be viewed in the context of clinical decision making for urgently ill patients. But the NEJM has a "just the facts, please" policy, which, in this case, leads to a false equivalency between ketamine and ECT, which will likely be detrimental to many of our most severely ill patients.
All ECT practitioners should read this article carefully and in full.
I am reminded of the quote from the infamous Lancet editorial of 1981: "It is not ECT which has brought psychiatry into disrepute. Psychiatry has done just that for ECT."
Let's see if NEJM will publish any critical LTEs.
(I will leave this post up as the latest one for a while, due to its importance.)



Comments
Post a Comment